Heart Failure and Pregnancy
Heart failure is a leading cause of health problems during and after pregnancy. Pregnancy causes changes in the body that place extra stress on the heart and circulatory system. For people with certain existing heart problems, pregnancy can increase the risk of heart failure. Pregnancy-related changes can also cause heart problems in people who have no prior history of heart disease.
-
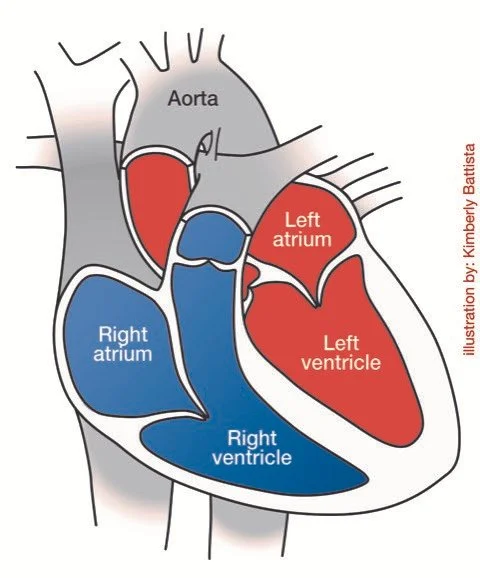
The heart is a muscle made up of four chambers with two pumps. The right side of the heart pumps blood to the lungs, where it picks up oxygen. The left side of the heart pumps blood to the body to deliver oxygen to all of your organs. Your organs need oxygen to function.
Heart failure occurs when the heart muscle is too weak or stiff to pump enough blood to meet the body’s needs. Heart failure may result from weakness of the heart muscle, damage to the blood vessels supplying the heart, structural abnormalities of the heart, or a problem in the heart’s electrical system.
-
Pregnancy naturally places extra stress on the heart and circulatory system to support the blood flow to the placenta and growing fetus. These changes include:
Increased amount of blood: The heart pumps more blood to deliver nutrients and oxygen to the fetus.
Increased heart rate: The heart beats faster than usual to handle the increased blood flow.
Lower blood pressure: Blood vessels relax and widen during pregnancy, causing a natural drop in blood pressure.
While these changes are usually manageable in a normal pregnancy, they can sometimes lead to heart failure, even in people without existing heart conditions.
-
Some of the most common causes of heart failure during pregnancy include:
Peripartum cardiomyopathy (PPCM): A condition where the heart muscle weakens, typically in late pregnancy or the months following delivery in a previously normal heart.
Preeclampsia: A pregnancy complication causing high blood pressure that can strain the heart.
Valvular heart disease: Abnormalities with the valves of the heart that can prevent blood from flowing normally through the heart.
Pulmonary hypertension: High blood pressure in the lung blood vessels that increases stress on the heart.
-
If you have a history of heart failure or any other heart condition, it is important to consult with your doctor before becoming pregnant. Your doctor will assess your risks to evaluate how safe pregnancy might be for you based on the severity of your heart condition. Understanding how pregnancy may affect your health is essential to making an informed decision.
In individuals with severe heart failure or significant heart disease, pregnancy may not be advisable. If you are already pregnant, your healthcare team will closely monitor your condition and discuss options for managing your health.
-
Heart failure can increase risks for both the pregnant person and the fetus. Symptoms like swelling, fatigue, and shortness of breath can worsen for the pregnant person, especially later in pregnancy. In severe cases, hospitalization may be necessary to manage symptoms.
For the fetus, reduced maternal blood flow can lead to complications such as preterm birth, fetal growth restriction (poor growth), or low birth weight, which can increase the risk of health problems after birth.
-
Heart failure during pregnancy is diagnosed by symptoms, a physical exam, and tests. Common symptoms include shortness of breath, leg swelling, and fatigue that worsens with activity.
Diagnostic tests may include:
Echocardiogram: An ultrasound of the heart to check how well it pumps blood
Blood tests to assess heart function and identify signs of stress or fluid buildup
Electrocardiogram (EKG): A test that checks the heart’s electrical activity
-
A team of healthcare providers and specialists will work together to manage your pregnancy, including a cardiologist and a maternal-fetal medicine (MFM) subspecialist. In some cases, you may be transferred to an advanced facility with multiple specialties. The team will monitor both your heart health and fetal development.
Your care plan may include:
Frequent monitoring: You will have regular check-ups to monitor heart function, symptoms, and overall health.
Medications: Specific medications may be prescribed depending on your heart condition. If you were taking medications before pregnancy, your healthcare team will evaluate whether they are safe to continue during pregnancy or if they need to be stopped or replaced.
Fetal monitoring: Regular ultrasounds will monitor your baby’s growth. A fetal echocardiogram may also be recommended to evaluate the fetal heart.
-
If your health is stable and the fetus is growing well, you should be able to deliver at term.
Your doctor may recommend delivering earlier in certain situations, including if your heart condition worsens, you develop preeclampsia, or the fetus is not growing as expected.
-
Your doctor may recommend delivery at a hospital with experience in caring for pregnant patients with heart failure. Most people with heart failure can have a safe vaginal delivery with careful monitoring. Vaginal delivery is generally preferred because it involves less strain on the heart compared with a cesarean delivery (C-section).
To minimize stress during the pushing stage of labor, your doctor may recommend assistance with forceps or a vacuum to help deliver the baby. Cesarean delivery may be necessary in specific medical situations. It is not routinely recommended for heart failure alone.
Pain management options, such as an epidural, are usually safe and can help reduce heart strain during labor. Your doctor will determine the best option for you based on your condition.
-
The postpartum period is a critical time for individuals with heart failure. Following delivery, blood and fluids in the body shift rapidly, which can overload the heart and circulatory system. After delivery, you will be closely monitored for signs of fluid overload or worsening symptoms. Medications that were paused or changed during your pregnancy may also be restarted at this time.
Follow-up care is essential once you leave the hospital. You should have a follow-up care plan in place before you are discharged and should see your cardiologist or primary care provider within 1-2 weeks after leaving the hospital to ensure your recovery is on track.
-
Yes, most people with a history of heart failure can breastfeed. Some medications, however, are not recommended during breastfeeding. Your healthcare team will review all of your medications and discuss what is known about their safety during breastfeeding so that you can make an informed decision.
Quick Facts
Heart failure is a leading health risk during pregnancy and can develop even in people with no prior heart disease.
Pregnancy increases the workload of the heart and circulatory system, which can worsen pre-existing heart disease or lead to heart failure for the first time.
Pre-pregnancy counseling and postpartum monitoring are essential for individuals with heart conditions to manage risks and ensure a safe recovery.
Heart failure is diagnosed through physical exams and tests, with regular monitoring to manage symptoms.
Heart failure increases the risk of pregnancy complications, such as preterm birth, fetal growth restriction, and low birth weight.
Treatment is individualized, often including medications tailored to your heart condition.
A team of specialists, including a cardiologist and MFM subspecialist, should guide your care during pregnancy and delivery.
Glossary
Cardiomyopathy: A disease of the heart muscle that reduces the heart’s ability to pump blood to the body.
Cesarean delivery (C-section): Surgery in which a baby is delivered through a cut (incision) in the mother’s uterus.
Circulatory system: The system of blood vessels that moves blood throughout the body. It brings oxygen to the body’s organs and removes waste products. Includes the heart, blood vessels, and lungs.
Dilated cardiomyopathy: A condition where the heart's left ventricle enlarges and weakens, reducing the heart's ability to pump blood effectively.
Echocardiogram: An ultrasound exam that checks the structure and function of the heart.
Electrocardiogram (EKG): A test that records the electrical activity of the heart to detect irregular heart rhythms and other cardiac problems.
Epidural: A type of anesthesia used during childbirth, where medication is injected into the epidural space in the spine to block pain in the lower part of the body.
Fetal echocardiogram: An ultrasound exam that checks the structure and function of the fetal heart.
Fetal growth restriction: A condition in which a fetus measures much smaller than expected for the gestational age.
Forceps: A medical instrument shaped like a pair of large spoons or tongs used to help deliver a fetus during vaginal childbirth.
Hypertension: A condition where the force of blood against the artery walls is too high, also known as high blood pressure.
Maternal-fetal medicine (MFM) subspecialist: An obstetrician with specialized training in caring for people with high-risk pregnancies.
Oxygen: The gas used by the human body to convert food into energy.
Peripartum cardiomyopathy (PPCM): A condition in which the heart muscle weakens and enlarges during the final stages of pregnancy or after childbirth.
Preeclampsia: A disorder that can occur during pregnancy in which the blood pressure gets too high. It can damage many organs in the body, including the kidneys, brain, and liver.
Preterm birth: Delivery of a baby before 37 weeks of pregnancy.
Pulmonary hypertension: High blood pressure that affects the arteries of the lungs (the pulmonary arteries) and the right side of the heart.
Ultrasound: Use of sound waves to create images of internal organs or the fetus during pregnancy.
Vacuum: A suction device applied to the fetus's head to help guide it out of the birth canal during vaginal delivery.
Ventricles: The two lower chambers of the heart that pump blood to the lungs (right ventricle) or the rest of the body (left ventricle).
Content Update: May 2025