Twin-Twin Transfusion Syndrome (TTTS) and Twin Anemia-Polycythemia Sequence (TAPS)
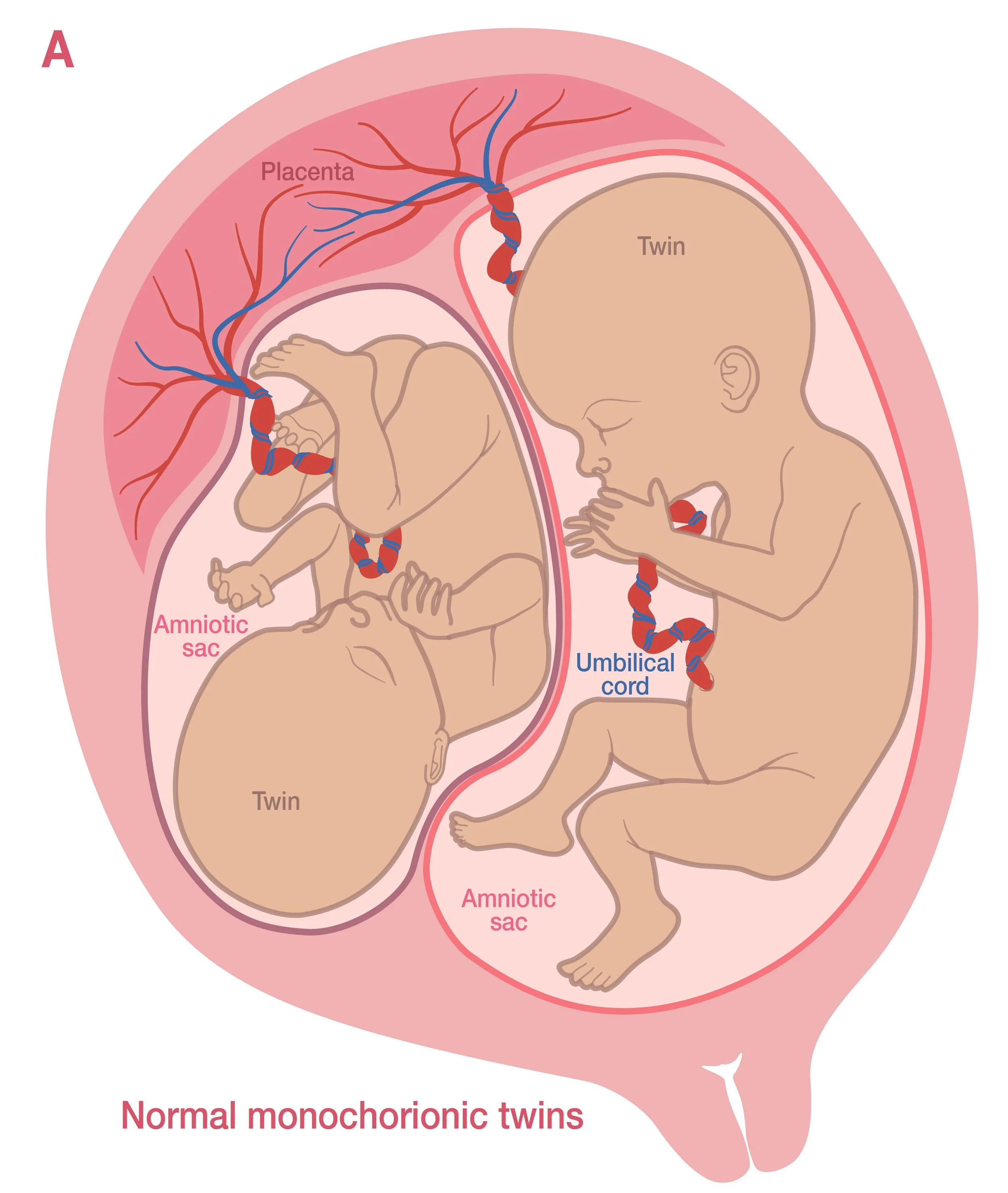
In a monochorionic (MC) twin pregnancy, the twin fetuses share a single placenta. In most MC pregnancies, each twin grows within its own amniotic sac. This is called a monochorionic diamniotic (MCDA) pregnancy. In rare cases, the twins grow within a single amniotic sac. This is called a monochorionic monoamniotic (MCMA) pregnancy.
In nearly all MC twin pregnancies, the twins’ blood circulations are joined at various points along the surface of the placenta. If blood flow between the twins becomes unbalanced, it can lead to twin-twin transfusion syndrome (TTTS) or twin anemia-polycythemia sequence (TAPS). These conditions may cause serious complications for both twins.
-
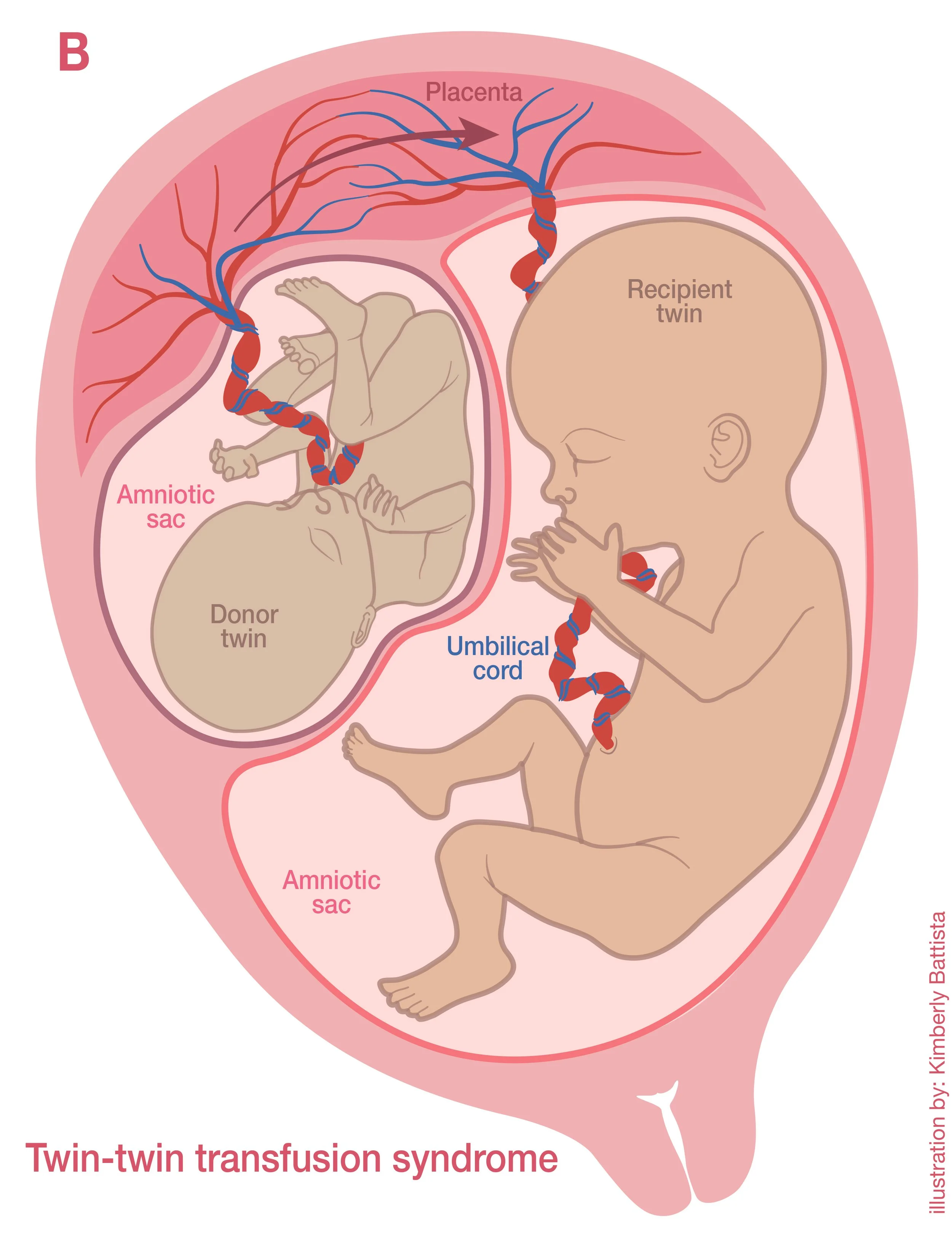
TTTS occurs when there is unequal sharing of blood between monochorionic (MC) twins.
One twin, called the donor twin, does not receive enough blood and fluids. This results in oligohydramnios (low amniotic fluid). Donor twins have problems growing, which can affect their overall health.
The other twin, called the recipient twin, receives extra blood and fluid from its co-twin. This results in polyhydramnios (high amniotic fluid). Recipient twins are at risk of heart failure or hydrops (an abnormal amount of fluid collecting in parts of the body where it should not be). See image below
Because TTTS affects organ development, it may result in the loss of one or both twins. Twins who survive can face lifelong health challenges, such as neurologic disabilities, including blindness, deafness, developmental delays, and cerebral palsy; heart defects; and kidney problems.
Prematurity is common in TTTS twins and can cause additional complications, including breathing issues, underdeveloped bones, brain abnormalities, digestive disorders, and vision or hearing loss.
-
A 5-stage system is used to describe the severity of TTTS. In general, higher stages of TTTS have less favorable outlooks. TTTS can worsen, improve, or stay the same at any stage but is less likely to improve at advanced stages.
-
TTTS is diagnosed with ultrasound. If you are pregnant with MCDA twins, you will have regular ultrasound exams to check for TTTS starting at around 16 weeks of pregnancy.
Since TTTS can develop at any time during pregnancy, ultrasound screening will continue until delivery.
-
Management depends on many factors, including gestational age (how far along the pregnancy is) and the TTTS stage. Options may include expectant management, fetal therapy if you are a candidate, amnioreduction in some cases, or termination of one or both twins (abortion). Depending on the geographic location and associated laws, abortion may not be offered.
You may be referred to a fetal care center for treatment. Fetal care centers provide specialized care for pregnant people with conditions that put them and the fetus(es) at a high risk of complications.
-
Fetoscopic laser surgery (FLS) is a type of minimally invasive surgery used to treat TTTS and other complications of twin pregnancies. It is usually offered between 16 and 26 weeks of pregnancy. It can sometimes be considered at earlier or later gestational ages. FLS is best performed at a fetal care center.
InFLS, a fetoscope (a long, specialized camera) is inserted through the mother’s abdomen and into the uterus into the recipient twin’s amniotic sac. A laser is then used to seal off the connections between the twins’ blood vessels. Sealing these connections stops the blood flow between the twins.
FLS is considered the best available treatment for early-onset, advanced-stage TTTS. Overall, when FLS is performed at a fetal care center:
Both twins survive in 50% to 70% of cases
1 twin survives in 20% to 30% of cases, and
None survive in 10% to 20% of cases.
-
Although FLS may treat TTTS, it comes with several risks:
Preterm premature rupture of membranes (PPROM). This is the most common complication of FLS. PPROM can cause serious health problems for a pregnant person, such as infection. For the fetus, PPROM can lead to stillbirth or preterm birth.
Placental abruption, in which the placenta separates from the wall of the uterus.
Fetal risks, including injury during the procedure and fetal death.
Twin anemia-polycythemia sequence (TAPS), another type of unbalanced blood flow that can develop after FLS (discussed below).
-
Preterm birth is common after FLS. One study found that, on average, people remained pregnant for about 10 more weeks following FLS, with most giving birth around 30 weeks of pregnancy.
Although most twins born after FLS have normal brain function, up to 1 in 5 have neurologic problems at 2 years of age. These deficits are likely related to being born preterm as well as to the TTTS itself.
-
In amnioreduction, a thin needle is inserted into the uterus to remove excess amniotic fluid. It is typically done under ultrasound guidance. Amnioreduction may be done when TTS is diagnosed later in pregnancy and fetal therapy is no longer an option.
-
TAPS occurs when one twin slowly loses blood to the other twin. TAPS causes one twin to have anemia (low red blood cell count) and the other twin to have polycythemia (high red blood cell count). TAPS can occur naturally or as a complication of FLS for TTTS.
The unbalanced blood flow can cause heart and neurological problems for both twins. There is also an increased risk of preterm birth and growth problems. Some twins with TAPS may not survive until birth. However, outcomes vary widely and are hard to predict.
-
TAPS may be identified during the second or third trimester of pregnancy or after birth. Before birth, Doppler ultrasound may be used to screen for the condition if it is suspected. TAPS often presents with additional ultrasound findings that can confirm the diagnosis.
After birth, TAPS may be suspected when there is a visible physical difference in the twins: one may be pale, and the other may have a ruddy or red-colored skin tone. Blood tests after delivery can confirm a diagnosis of TAPS when there is suspicion that it is present.
-
Many options can be considered when managing TAPS. Care decisions are often made on a case-by-case basis. Management depends on gestational age, the severity of the condition, technical considerations, and whether other fetal or maternal concerns are present. Close monitoring is usually recommended for mild cases of TAPS diagnosed before 32 to 34 weeks. After 32 to 34 weeks, delivery may be recommended. If TAPS is diagnosed after birth, the baby may need specialized pediatric care.
For more severe cases of TAPS diagnosed in the second or third trimester before 32 weeks, you may be referred to a fetal care center. Potential management options that may be offered include FLS, intrauterine blood transfusion therapy, or delivery. Abortion may be considered in rare cases.
-
As with TTTS, newborns who survive TAPS have a similarly increased risk of neurologic problems. They may also have long-term health issues due to being born preterm or from the effects of TAPS on developing organs.
Quick Facts
In twin pregnancies where the fetuses share a placenta, twin-twin transfusion syndrome (TTTS) and twin anemia-polycythemia sequence (TAPS) are potential complications that both involve uneven sharing of blood between the fetuses.
TTTS can be detected through regular ultrasounds starting at 16 weeks of pregnancy.
TAPS can be identified before birth using Doppler ultrasound, after birth by visible physical differences in the twins, or by a blood test.
Both TTTS and TAPS can lead to serious health complications for the twins or even fetal death and may require specialized care.
TTTS or TAPS patients may be referred to a fetal care center for expert evaluation and treatment.
Fetoscopic laser surgery (FLS) may be a treatment option for TTTS and TAPS. For TTTS, FLS is typically performed between 16 and 26 weeks of pregnancy.
Glossary
Abortion: Taking medication or having a medical procedure to end a pregnancy so that it does not result in a live birth.
Amnioreduction: A procedure in which excess amniotic fluid is removed from the uterus during pregnancy.
Amniotic fluid: The fluid surrounding the fetus in the uterus that is essential for the fetus’s growth and development.
Anemia: A condition where the body has a lower-than-normal number of red blood cells.
Cerebral Palsy: A group of disorders caused by brain damage or abnormal brain development that affect balance, posture, and movement.
Doppler ultrasound: A specialized type of ultrasound exam that measures blood flow through a blood vessel.
Expectant management: A course of care in which the healthcare provider closely monitors a patient's condition without immediately intervening with active treatment.
Fetal therapy: Medical or surgical interventions during pregnancy to diagnose, manage, or treat conditions affecting the fetus.
Fetus: The unborn offspring of a human that develops in the uterus; the fetal stage lasts from nine weeks to birth.
Fetoscopic laser surgery (FLS): A minimally invasive procedure using a camera and laser to treat certain fetal conditions by sealing abnormal blood vessels in the placenta.
Gestational age: The age of a pregnancy, usually given in weeks. A pregnancy is dated from the first day of the last menstrual period. The standard length of pregnancy is 40 weeks.
Hydrops: An abnormal amount of fluid collecting in parts of the body where it should not be.
Minimally invasive surgery: A type of surgery involving very small incisions or no incision at all, resulting in reduced tissue damage and scarring.
Monochorionic-diamniotic (MCDA) pregnancy: Identical twins who develop in their own amniotic sacs but share a placenta.
Monochorionic-monoamniotic (MCMA) pregnancy: Identical twins who develop in one amniotic sac and share a placenta.
Oligohydramnios: Low amniotic fluid during pregnancy.
Oxygen: The gas used by the human body to convert food into energy.
Placenta: A special organ that develops during pregnancy. It allows the transfer of nutrients, antibodies, and oxygen to the fetus. It also makes hormones that sustain the pregnancy.
Placental abruption: A condition where the placenta separates from the wall of the uterus.
Polycythemia: Having a higher number of red blood cells than normal.
Preterm premature rupture of membranes (PPROM): A complication of pregnancy in which the amniotic sac breaks before 37 weeks of pregnancy.
Intrauterine blood transfusion: A procedure in which donor blood is given to the fetus before birth.
Twin anemia-polycythemia sequence (TAPS): A condition in which twins who share a placenta receive unequal amounts of red blood cells.
Twin-twin transfusion syndrome (TTTS): A condition in which twins who share a placenta receive uneven amounts of blood, oxygen, and nutrients.
Ultrasound: Use of sound waves to create images of internal organs or the fetus during pregnancy.
Uterus: The organ in which the fetus develops during pregnancy.
Last Updated: March 2025